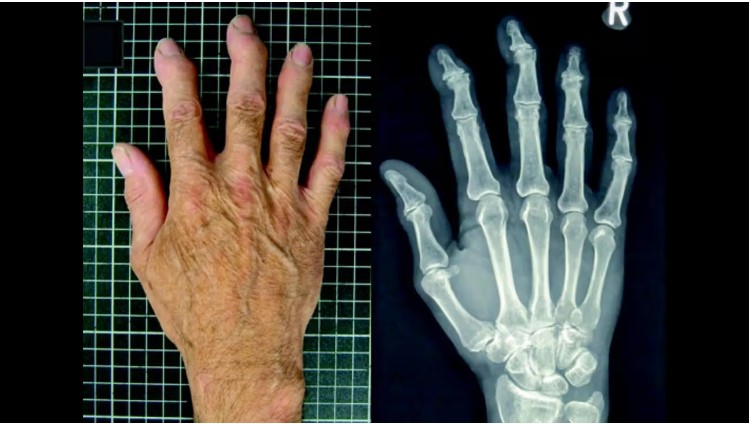
Erosive osteoarthritis is a specific type of osteoarthritis that predominantly affects the fingers. Common symptoms include pain, swelling, warmth, and redness. Women around the age of 50 are most at risk, potentially due to the loss of estrogen.
As a type of inflammatory osteoarthritis, erosive osteoarthritis typically develops in the hinge joints of the fingers and less frequently in the toes. Clinically, these joints are referred to as the interphalangeal joints.
Research suggests that less than 3% of the population develops erosive osteoarthritis. Approximately 10% of individuals with symptomatic osteoarthritis suffer from this inflammatory joint condition.
Erosive osteoarthritis can lead to:
- Subchondral sclerosis, or hardening of the bone near the cartilage
- Narrowing of the space between bones
- Erosions, or the destruction of some bone material
What Are the Symptoms of Erosive Osteoarthritis?
Diagnosing erosive osteoarthritis can be challenging for doctors, even with the use of X-rays and other imaging tests. An analysis of numerous studies found that there can be disagreement among doctors regarding which joint changes indicate erosive osteoarthritis.
One widely accepted sign of the condition is its sudden onset. While stiffness and soreness associated with conventional osteoarthritis tend to develop gradually, symptoms of erosive osteoarthritis usually appear without warning.
These symptoms primarily affect the fingers and generally include:
- Sudden-onset pain
- Swelling
- Warmth
- Redness
- Reduced hand function (making it harder to grip objects, for example)
Joint function changes usually occur in the proximal joints (the middle of the fingers) rather than the distal joints (near the fingertips).
What Causes Erosive Osteoarthritis?
Health experts remain divided on whether erosive osteoarthritis is an aggressive form of osteoarthritis or an entirely distinct type of arthritis.
Typical osteoarthritis results from wear and tear on the joints over time or from injuries that don’t heal properly. Erosive osteoarthritis, however, does not share these origins. Researchers believe hormones may play a role, given that the condition more frequently affects women than men.
Another possibility is that erosive osteoarthritis could be linked to an autoimmune condition.
Who Is at Risk for Erosive Osteoarthritis?
Erosive osteoarthritis predominantly affects women around the age of 50. Researchers speculate that the loss of estrogen may contribute to this, especially since typical osteoarthritis of the hands and knees is much more common in individuals after menopause.
A family history of erosive osteoarthritis also increases the risk of developing the condition.
Additionally, the presence of conventional osteoarthritis may elevate the risk. The estimated prevalence of erosive osteoarthritis in the general population is less than 3%, but this rate climbs to approximately 10% among people with symptomatic hand osteoarthritis.
For perspective, the CDC reports that nearly 50% of individuals aged 65 and older have been diagnosed with some form of arthritis.
It is also noteworthy that women are diagnosed with arthritis more frequently than men.
How Is Erosive Osteoarthritis Diagnosed?
The symptoms of erosive osteoarthritis, such as painful and swollen fingers, can resemble those of rheumatoid arthritis (RA) and psoriatic arthritis, both of which can also start in the fingers. Consequently, it is sometimes initially misdiagnosed.
However, an important distinction is that erosive osteoarthritis usually does not affect the wrist or the joints where the fingers meet the palm, which are common areas affected by RA.
To diagnose erosive osteoarthritis, a doctor will begin with a comprehensive review of the patient’s symptoms, personal medical history, and family medical history. Imaging tests play a crucial role in confirming the diagnosis. One diagnostic indicator is the presence of subchondral cysts or geodes in the fingers, resulting from the destruction of cartilage and bone in the joints.
Another distinguishing feature of erosive osteoarthritis, compared to standard osteoarthritis, is the presence of bone erosion.
How Is Erosive Osteoarthritis Managed or Treated?
There is currently no cure for erosive osteoarthritis, and it is a progressive, irreversible condition. The primary aim of treatment is to manage symptom severity and maintain joint function.
Many treatments for erosive osteoarthritis are similar to those for standard osteoarthritis. The severity of the symptoms will determine the most appropriate treatment approach.
NSAIDs and Analgesics
Over-the-counter and prescription-strength pain relievers are typically the first-line treatments for erosive osteoarthritis.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil), can help reduce the inflammation associated with the condition.
Analgesics, including acetaminophen (Tylenol), are effective pain relievers, especially for individuals who cannot tolerate NSAIDs.
Steroid Injections
Steroid injections aim to reduce inflammation and pain, but they can only be administered to an individual joint a few times a year. Typically, they are more effective in temporarily easing symptoms in larger joints, such as the knee or shoulder, rather than in the smaller joints of the hand.
Occupational Therapy
When finger and hand function become impaired, basic tasks like buttoning a shirt or using eating utensils can become challenging. An occupational therapist can teach you modified ways to perform everyday tasks independently or with the help of special tools and devices.
Occupational therapists encourage people with erosive osteoarthritis to engage in exercises designed to strengthen the affected joints and improve their function.
Heat Therapy
The use of hot compresses or hot water soaks is a mainstay of arthritis treatment. Heat helps dilate blood vessels, delivering more oxygen and nutrients to the tissues of your joints, thereby easing stiffness and relieving pain.
Heat therapy can be an effective complement to oral medications and other treatments.
What’s the Outlook for People with Erosive Osteoarthritis?
Living with erosive osteoarthritis may involve using a variety of therapies to manage symptoms and retain the use of your hands.
While there is no cure, the medical community increasingly acknowledges the need for greater research to better understand the origins of erosive osteoarthritis and to identify effective treatments.
Despite the pain and frustration that this condition can cause, being proactive and adhering to your treatment plan can help you maintain a good quality of life.
Erosive Osteoarthritis vs. Similar Conditions
Most types of arthritis involve some degree of joint pain, swelling, and stiffness. However, there are distinctions that can help you and your doctor determine which specific condition is causing your symptoms.
Erosive Osteoarthritis vs. Traditional Osteoarthritis
Erosive osteoarthritis typically produces more pain, swelling, and functional disability in the affected joint compared to traditional osteoarthritis. It also involves the erosion or destruction of bone.
In contrast, traditional osteoarthritis primarily involves the loss of cartilage and commonly affects the base of the thumb joint, a site typically not impacted by erosive osteoarthritis.
Erosive Osteoarthritis vs. Rheumatoid Arthritis
Rheumatoid arthritis often begins in the hands but usually involves other joints as well, such as the wrists and elbows. In contrast, erosive osteoarthritis is typically isolated to the fingers, though it can sometimes affect the toes.
Additionally, most people with RA test positive for specific biomarkers, including anti-cyclic citrullinated peptide (anti-CCP) antibodies, whereas individuals with erosive osteoarthritis usually test negative for these antibodies.
Erosive Osteoarthritis vs. Psoriatic Arthritis
Distinguishing between erosive osteoarthritis and psoriatic arthritis can sometimes be challenging if there are no signs of psoriasis, which manifests as a scaly rash on the skin.
In rare cases, people with psoriatic arthritis may develop painful arthritis symptoms before any dermatological changes occur. Once a psoriasis diagnosis is established, it becomes easier for your doctor to rule out erosive osteoarthritis as the cause of your symptoms.
